Wayne County Speech-Language Guidelines

Wayne RESA, in collaboration with local district representatives, has put together information on the following topics regarding speech and language services in Wayne County. Included in this page's accordions below are guidance information, forms, and links to frequently asked questions (FAQ).
Resources
These resources were compiled from a variety of sources including:
American Speech-language Hearing Association (ASHA)
Guidelines for Speech & Language Evaluation, Eligibility and Service Delivery in Schools (MSHA, 2025)
Kent County ISD Speech and Language Evaluation, Eligibility and Service Guidelines (2021)
Michigan Administrative Rules for Special Education (MARSE) With Related IDEA Federal Regulations
Michigan Speech Language Guidelines (2006)
Caseload / Workload and Service Delivery
Overview
Per MARSE R 340.1745, all of the following provisions are specific requirements for speech and language services:
- The speech and language services provided by an authorized provider of speech and language services shall be based on the needs of a student with a disability as determined by the individualized education program team after reviewing a diagnostic report provided by an authorized provider of speech and language services.
- The determination of caseload size for an authorized provider of speech and language services shall be made by the authorized provider of speech and language services in cooperation with the district director of special education, or his or her designee, and the building principal or principals of the school or schools in which the students are enrolled. Caseload size shall be based upon the severity and multiplicity of the disabilities and the extent of the service defined in the collective individualized education programs of the students to be served, allowing time for all of the following:
- (i) Diagnostics
- (ii) Report writing
- (iii) Consulting with parent/guardians and teachers
- (iv) Individualized education program team meetings
- (v) Travel
- Individual caseloads of authorized providers of speech and language services shall not exceed 60 different persons and shall be adjusted based on factors identified in subdivision (b) of this rule. Students being evaluated shall be counted as part of the caseload.
Workload vs. Caseload
Workload refers to all activities required and performed by school-based SLPs and other professionals. Caseload (or the number of students served) is just one part of the SLP's workload. Reasonable workloads allow for optimal service delivery to students to meet their individual needs as required under IDEA. The workload analysis approach is explained in ASHA's Caseload and Workload Practice Portal resource. See also ASHA’s Implementation Guide: A Workload Analysis Approach for Establishing Speech-Language Caseload Standards in Schools.
In order to be compliant with MARSE, ensure students receive FAPE, and achieve positive outcomes, thoughtful analysis of a SLP’s workload must be balanced by:
- severity and multiplicity of the disabilities on the caseload
- required activities such as diagnostics, documentation, consulting with parent/guardians and teachers, IEP team meetings, travel between buildings
- district and/or building level responsibilities
Additional activities such as building level universal supports and intervention, child study/MTSS/RtI participation, staff/family consultation/training, etc., which are outside of evaluating and providing services to students with IEPs, should be considered when determining caseloads.
Service Delivery
Using evidence-based decision making, SLPs have the responsibility to select the most appropriate service delivery model. Models should be chosen which afford the most flexible and efficient delivery of services; services should be outcome oriented, curriculum-based, and designed to improve the student’s ability to access and make progress in the general education curriculum. Combining service delivery models allows the SLP to focus on the individual needs of students, ensure the educational relevance of speech-language services, and reflect on treatment effectiveness. IDEA mandates that services be provided in the least restrictive environment and/or most natural setting, which can include the classroom or an alternate setting. Services can be provided in a variety of formats including, as outlined by ASHA.
- Traditional Weekly Schedule
- Receding Schedule
- Cyclical Schedule
- Block Schedule
- Blast or Burst Schedule
- Group Size
Least Restrictive Environment
To the maximum extent possible, students with disabilities must be educated with their non-disabled peers. This is referred to in IDEA as Least Restrictive Environment (LRE). Providing speech and language services in the classroom helps with generalization of the student's skills and provides additional opportunities for the SLP and classroom teacher to collaborate. This aids in developing the classroom teacher's awareness of the student's communication needs and strategies. Additionally, working in the classroom increases the SLP's awareness of the impact that curricular activities have on the student in order to develop appropriate strategies and plan of treatment. The SLP and classroom teacher having this open communication and mutual understanding of the student, and their needs, allows for adjustments in services to be driven by changes in classroom expectations, activities and curriculum.
Additional Resources
Caseload and Workload (ASHA)
Implementation Guide: A Workload Analysis Approach for Establishing Speech-Language Caseload Standards in Schools (ASHA)
School-Based Service Delivery in Speech-Language Pathology (ASHA)
Evaluation / Eligibility Overview
Eligibility
Speech-Language Impairment (SLI), as defined in MARSE 340.1710 (PDF) pg. 35-36, can be a primary or secondary eligibility. Since an adverse educational impact is required in one or more of the following areas: language, articulation, fluency, and/or voice, considerations should be given to academic, vocational and social-emotional aspects of a speech-language impairment. The following non-exhaustive list has examples of impact in each area. Informed clinical opinion, IEP team input, and student input must be included when determining the presence of an adverse educational impact.
Academic Impact
Students may have difficulty with:
Reading, math, and language arts with the impact determined by grades
Language-based activities
Comprehending information from text or orally presented
Conveying information orally
Decoding, sound/letter correspondence, encoding
Phonological awareness
Reading fluency
Solving math word-problems
Putting thoughts into writing
Telling stories or relating personal narratives in sequence
Being understood during checks for understanding/classroom assessments
Social-Emotional Impact
Students may have difficulty with:
Being understood by others
Peers teasing the student
Maintaining and terminating verbal interactions
Making and maintaining friendships
Embarrassment and/or frustration
Ability to express emotions and feelings related to social situations and/or during conflict resolution
*If a student does not experience a negative perception of their own speech, they may not benefit from treatment at that time.
Vocational Impact
Job-related skills that the student cannot demonstrate due to the SLI:
Understand/follow oral directions
Inappropriate responses to coworkers’ or supervisors’ comments
Inability to answer/ask questions in a coherent and concise manner
Difficulty being understood when speaking
Standard Evaluation Process
Prior to evaluating a child for a speech and language impairment, it is highly recommended that the district’s Multi-Tiered System of Support (MTSS) has been thoroughly reviewed. When evaluating a student for a Speech Language Impairment, the standard practice in Michigan for many years has been to qualify students who have test scores of 1 and 1/3 standard deviations below the mean, or standard scores of 80 or below. While this may continue to be observed as best practice, we recommend that tests are selected with appropriate sensitivity and specificity levels (>80%). Review the specific standardized test manual to review their recommended cut-off score. Remember, that a single test criterion should not be the sole determining factor for decisions. This document provides suggested practices and should not be interpreted as mandatory or as a means to supplant or replace the IEP team decision making process. SLPs should discuss and confirm their own district policies. For a comprehensive list of Speech and Language assessments refer to this Test Comparison Chart from Kent ISD’s Speech and Language Evaluation, Eligibility and Service Guidelines (March 2021).
Additional Resources
Michigan Administrative Rules for Special Education (MARSE) With Related IDEA Federal Regulations
Cognitive Referencing
Test Comparison Chart
Considerations When Discussing Discontinuation / Revocation of Services
Standard Speech and Language Evaluation Process Components
Bell Curve Handout
Bilinguistics Free Assessment Materials
Case History Form
Checklist for Reviewing Norm-Referenced Tests
Communication Matrix
Dynamic Assessment Goals Grid-3 (DAGG-2)
Elementary Informal Language Sample Checklist
FAQ Speech Sound Disorders for input forms relating to speech sound disorders
FAQ Language for input forms relating to language
FAQ Fluency for input forms relating to fluency
Fluency Speech Sample Form
MARSE ASD Eligibility Observation Form
MARSE ASD Eligibility Observation From (Preschool)
Oral Peripheral Mechanism Exam
Screening Report Form
School-age Language Assessment Measures (SLAM)
SETT Framework
SETT Framework - Joy Zabala, Ed.D.
Creator of the SETT Framework
The Rainbow Passage
Voice Input Forms relating to voice
Speech Sound Disorders: Articulation and Phonology
 Overview
Overview
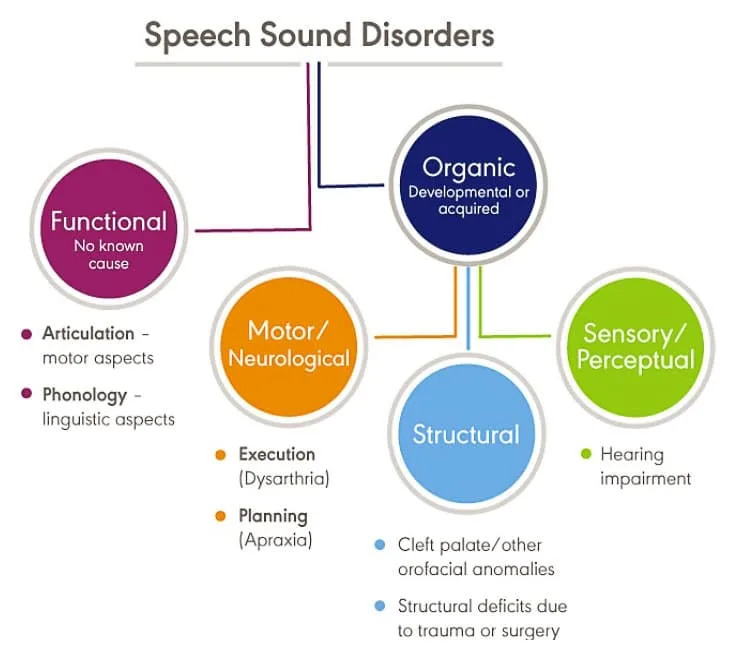
The purpose of this document is to support school teams in understanding and identifying speech sound disorders in students ages 0-26 years to support consistency in services throughout Wayne County. This document will cover the evaluation process, service delivery models, exit criteria, and definitions. Speech sound disorders is an umbrella term encompassing any difficulty or combination of difficulties with perception, motor production, or phonological representation of speech sounds and speech segments.
When a teacher or parent/guardian has concerns about a student’s articulation, consultation should occur with a SLP. After consultation, if the errors in articulation may be resolved without SLP intervention, then the SLP could suggest strategies for the student, teacher, and parent/guardians to use. If the student needs additional intervention support, they may receive that support through your district's MTSS process. If the student begins to progress, interventions/suggestions will continue to be used as needed by the teacher and/or parent/guardians. When there is appropriate student progress in response to the intervention, no referral is necessary. If it is determined that the student is not making appropriate progress based on data collected, the special education evaluation process may be initiated by the parent or service providers to meet and complete the REED document.
Evaluation & Eligibility
On top of the standard evaluation procedures, additional regarding speech sound disorders are:
- areas of assessment by years of age:
- 0-3: Intelligibility, syllable shapes, vowel sound production
- 3-5: Intelligibility, phonological processes & stimulability are the primary focus
- 6-9: Speech sound production norms & stimulability are the typical focus. Social and academic variables should be given stronger consideration at this age.
- 9+: Stimulability and social/academic/vocational considerations are of high importance for this age group
- Intelligibility Norm Chart
- Articulation Norms for typical age consonant sound is acquired
- Crowe and McLeod (2020) articulation norm chart is a conservative perspective
- Goldman Fristoe (2015) is a more liberal perspective
Informed clinical opinion should be derived from multiple sources of information. Test scores and standard deviations should not be the sole criterion for determining eligibility. The suspected disability must adversely affect educational performance (socially, academically and/or functionally). With speech sound disorders, the number of errors as well as the Speech Sound Production Severity Rating Scale should be qualifying factors.
Additionally, speech sound disorders may signal problems with phonological skills that affect spelling, reading and writing. For more examples please see the Eval/Eligibility one-pager. Some additional resources are linked below:
Service Delivery
The SLP should strive to design a speech intervention program that involves daily opportunities (either in the therapy, classroom, or home setting) for the student to practice with materials that are relevant to the curriculum for the generalization of speech. The SLP can collaborate with the classroom teacher to utilize strategies and or materials which provide the student speech practice that is relevant to his or her education.
Frequency should be aligned with severity and individual student needs as determined by the IEP team. For assistance with determining service delivery, please refer to the Severity/Intervention Matrix for Speech and Language Services from ASHA.
Exit Criteria
The determination of dismissal, For a student that qualifies for SLI due to a speech sound disorder, should consider that current best practice research suggests that students who are dismissed at 75- 85% accuracy in conversational speech often go on to fully correct, suggesting that this is an appropriate time for dismissal, in addition to the general exit considerations. Based on guidelines from Michigan Speech-Hearing Association (MSHA) and American Speech-Language Hearing Association (ASHA), speech-language services should be discontinued when there is minimal progress documented over “one to two consecutive years” due to the ineffectiveness of continued services since limited to no benefit can be reasonably expected. If a student has made minimal measurable progress and a lengthy plateau of articulation abilities despite program modifications and varied approaches, dismissal from speech-language services should be considered by the IEP team to ensure that the student has access to a free appropriate public education (FAPE) to the maximum extent possible.
Input forms: Student, Parent and Teacher
Speech Sounds - Student Input
Speech Sounds - Parent Input
Speech Sounds - Teacher Input for K-2nd Grade
Speech Sounds - Teacher Input for 3rd-5th Grade
Speech Sounds - Teacher Input for Middle School
Speech Sounds - Teacher Input for High School
Additional Resources
Intelligibility Norm Chart
Crowe and McLeod (2020) - Articulation norm chart is a conservative perspective
Goldman Fristoe (2015) - Articulation norm chart from a more liberal perspective
Speech Sound Production Severity Rating Scale
Phonological Processes Chart
Oral Peripheral Mechanism Exam
Frequently Asked Questions - Speech Sound Disorders
Language
Overview
When a teacher and/or parent/guardian has concerns about a student’s language development, the student should be brought to the school’s student success/child study team to discuss needs and concerns. General education interventions (RtI, observations, data gathering) should be put in place unless Child Find is triggered. In the case where the parent/guardian has requested an evaluation, the team would complete a REED. If interventions do not indicate progress, the team must proceed with a formal evaluation.
Language impairment is the inadequate or inappropriate acquisition, comprehension or expression of language. Language impairments can affect spoken, written, and/or use of an AAC system. Both expressive and receptive language impairments are divided into three categories: Form (Phonology, Morphology, Syntax), Content (semantics), and Use (Pragmatics). See the language impairments chart in FAQ language document for more information. Students who have Limited English Proficiency (LEP) or those students who are not speakers of Standard American English due to sociocultural dialects are not automatically considered to be students with a speech-language impairment. The presence of a language impairment does not necessarily guarantee the student’s eligibility for special education.
While MARSE criteria utilizes the terminology “Speech and Language Impairment” (SLI) as an eligibility category, SLPs should be familiar with the growing use of the term Developmental Language Disorder (DLD). According to ASHA, Children with DLD (in which language difficulties are not associated with a known biomedical condition) can coincide with impairments in the areas of attention, motor coordination, literacy, speech, behavior or emotional problems, executive function, or auditory processing.
Evaluation And Eligibility
When assessing for a language impairment, the SLP must determine whether any difficulty exists in a student’s ability to understand and use language effectively in the areas of phonology, morphology, syntax, semantics, and/or pragmatics. Inadequate language functioning must be demonstrated on both a language sample and at least 2 standardized assessments or subtests for a student to qualify as a student with a speech-language impairment MARSE Guidelines (page 36).
Parent/guardian consent must be obtained to begin the formal gathering of data on a student. This is done through the REED process in which current information is gathered and a team decides what further information is needed. According to ASHA, a comprehensive language assessment would include the following components:
- Standardized Assessment
- Discourse Assessments
- Language Sampling
- Narrative Sampling
- Dynamic Assessment
- Systematic Observation/Contextual Analysis
- Parent/Guardian/Teacher/Student Report Measures
- Language Diversity
- Language severity ratings
The SLP and IEP team gather information from the comprehensive assessment and proceed to summarize information within the evaluation report. The team must consider whether the assessment results support the identification of a language impairment. In order to do so, the team must address adverse educational impact, limited English proficiency, and cultural/linguistic differences. Adverse impact should be considered when determining eligibility. The team must determine how language deficits adversely impact the student’s education when compared to same age/grade peers. Gathering teacher, parent/guardian, and student input can be helpful here. See the Language Severity Rating Scale to help determine student language functioning.
Service
Curriculum Based Services are important to consider, especially when addressing a language impairment. Adverse impact and teacher input can be a helpful starting point for intervention/goal targets, as well as Common Core Standards and Early Childhood Standards of Quality. Because of the global nature of a language impairment, modifications and accommodations of the curriculum may be considered in order to meet student language needs across all academic settings. Any accommodations that the student requires within their academic settings must be indicated within the IEP. This includes universal accommodations that the student relies on to be successful. Delivery of accommodations listed in this section must be documented. The IEP Team determines which service delivery options will be employed to accomplish goals and objectives. The options should be reviewed and changed over time, as the student’s needs change.
Exit Considerations
For a student that qualifies for SLI due to a language disorder, in addition to the general Exit Considerations, dismissal should be considered if the student’s language needs have been resolved or are being met through specialized instruction or support provided with resource or self-contained programming.
Language Impairments
| Spoken Language Impairment | Listening (Receptive) | Speaking (Expressive) |
|---|---|---|
| Phonology | ability to identify and distinguish phonemes while listening (i.e., phonological awareness) | appropriate use of phonological patterns while speaking |
| Morphology | understanding morphemes when listening | using morphemes correctly when speaking |
| Syntax | understanding sentence structure elements when listening | using correct sentence structure elements when speaking |
| Semantics | listening vocabulary | speaking vocabulary |
| Pragmatics (includes discourse) | understanding of the social aspects of spoken language, including conversational exchanges | social use of spoken language, including production of cohesive and relevant messages during conversations |
| Written Language Impairments | Reading | Writing |
|---|---|---|
| Phonology | understanding of letter-sound associations while reading (i.e., phonics) | accurate spelling of words while writing |
| Morphology | understanding grammar while reading | appropriate use of grammar when writing |
| Syntax | understanding sentence structure while reading | using correct sentence structure when writing |
| Semantics | reading vocabulary | writing vocabulary |
| Pragmatics (includes discourse) | understanding point-of-view, needs of the audience, etc. | conveying point-of-view, intended message, etc. |
Input Forms: Student and Teacher
Language - Student Reflection
Language - K-2 Teacher Input
Language - 3-5 Teacher Input
Language - Middle School Teacher Input
Language - High School Teacher Input
Fluency
Overview
 When a teacher and/or parent/guardian have concerns regarding a student’s speech fluency, they should consult with a SLP to determine if further assessment is necessary. If the team feels that with consultation from the SLP, the disfluency may be resolved, the SLP suggests strategies for the parent/guardian, student, and teacher to use and then follows up periodically. If the disfluencies persist, then a speech-language evaluation may be necessary.
When a teacher and/or parent/guardian have concerns regarding a student’s speech fluency, they should consult with a SLP to determine if further assessment is necessary. If the team feels that with consultation from the SLP, the disfluency may be resolved, the SLP suggests strategies for the parent/guardian, student, and teacher to use and then follows up periodically. If the disfluencies persist, then a speech-language evaluation may be necessary.
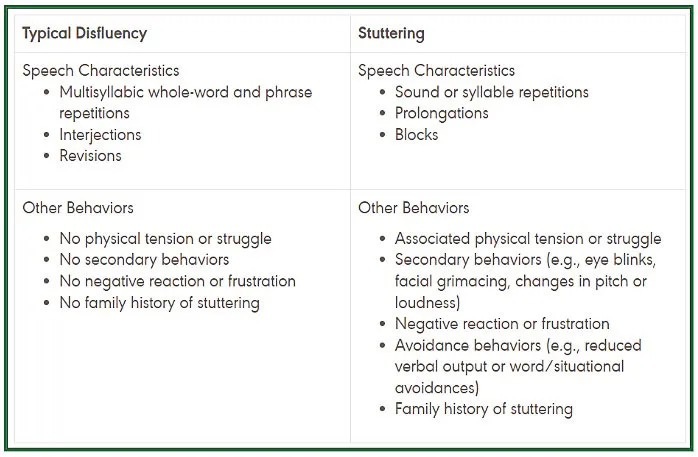
Definitions
Stuttering is an interruption in the flow of speaking characterized by repetitions (sounds, syllables, words, phrases), sound prolongations, blocks, interjections, and revisions, which may affect the rate and rhythm of speech. These disfluencies may be accompanied by physical tension, negative reactions, secondary behaviors, and avoidance of sounds, words, or speaking situations.
Cluttering is a disorder of speech and language processing resulting in rapid, dysrhythmic, sporadic, unorganized, and frequently unintelligible speech. Accelerated speech is not always present, but an impairment in formulating language almost always is.
Evaluation & Eligibility
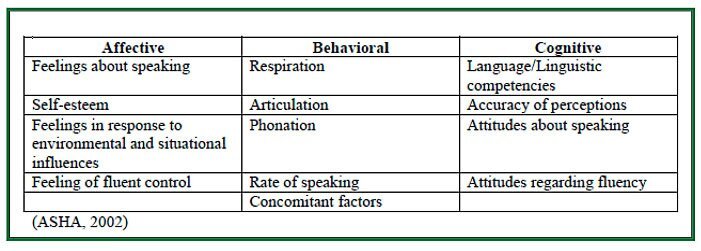 Based on the information gathered, the team decides whether the student is experiencing an adverse educational effect as a result of a fluency disability. Educational success involves academic, social, behavioral and emotional success. Thus, if the child is limiting class participation, has reduced interaction with others, speaking or situational fears, or expresses concern about stuttering, assessment and intervention are indicated.
Based on the information gathered, the team decides whether the student is experiencing an adverse educational effect as a result of a fluency disability. Educational success involves academic, social, behavioral and emotional success. Thus, if the child is limiting class participation, has reduced interaction with others, speaking or situational fears, or expresses concern about stuttering, assessment and intervention are indicated.
Several risk factors are reported to increase the likelihood that a student will continue to stutter (See FAQ). The SLP should consider these risk factors when determining whether to intervene informally or to expedite the formal assessment and treatment process as the more risk factors evident, the higher probability that the student will continue to struggle with fluency.
Service Delivery
The IEP Team determines which service delivery option(s) will be used to meet the student’s needs and accomplish IEP goals. Service is determined by need, and intervention should be designed to help the student increase participation and make progress in the general education curriculum. For assistance with determining service delivery, please refer to ASHA’s School-Based Service Delivery in Speech-Language Pathology (WEB) and Severity/Intervention Matrix for Speech and Language Services.
Exit Considerations
For a student that qualifies for SLI due to a fluency disorder, in addition to the general Exit Considerations, benchmarks for success should not be based solely on the frequency of stuttering. For example, a student who stutters more frequently may be less impacted by stuttering than a student who stutters less. The amount of impact may be dependent on the severity of disfluencies (e.g. blocks versus whole word repetitions), length of disfluencies, presence of secondary behaviors, and student’s feelings regarding stuttering. See FAQ for additional information about exit considerations.
Input forms: Student, Parent and Teacher
- Fluency - Student Input (K-4th)
- Fluency - Student Input
- Fluency - Parent Input
- Fluency - K-2 Teacher Input
- Fluency - Upper Elementary Teacher Input
- Fluency - Middle School Teacher Input
- Fluency - High School Teacher Input
Fluency Severity Rating Scale
- Severity Rating Scale from Kent ISD Speech and Language Evaluation, Eligibility and Service Guidelines Appendix
Voice
Overview
When students present with laryngitis or hyponasality, a brief conversation about the duration, symptoms and possible presence of a cold or allergies can alleviate concern. If the team feels that with consultation from the SLP, the vocal quality may be resolved, the SLP then suggests strategies for the student, teacher and parent/guardian to use. If there appears to be vocal quality that adversely affects the student’s educational performance which needs direct intervention from the SLP, then a REED process will begin and parent/guardian consent for an evaluation will be obtained. A request for a medical evaluation, such as a visit to an otolaryngologist (ENT), may occur during the referral or evaluation process.
Definitions
Voice disorder occurs when voice quality, pitch, and loudness differ or are inappropriate for an individual's age, gender, cultural background, or geographic location. A voice disorder is present when an individual expresses concerns about having an abnormal voice that does not meet daily needs, even if others do not perceive it as different or deviant. A number of different systems are used for classifying voice disorders.
Evaluation & Eligibility
Based on the information gathered, the team decides whether the student is experiencing an adverse educational effect as a result of a voice disability. Educational success involves academic, social, behavioral and emotional success. A comprehensive evaluation should consider input from the student, teacher and parent/guardian; and the following:
- Vocal Quality - Assess the student’s vocal characteristics looking for difficulties such as breathiness, stridency, or hoarseness. Breath supply should be evaluated for the amount and efficiency of air to sustain speech. Phonatory efficiency should be evaluated to assess the student’s ability to sustain quality phonation. Muscle tension during speech production should also be evaluated looking for signs of hypertension, hypotension, and anxiety when speaking.
- Pitch - Assess the student for difficulties such as extraordinarily high or low pitch, pitch breaks, or monotone.
- Loudness - Assess the student for difficulties such as excessive loudness or softness.
- Resonance - Resonance disorders are usually the result of a variety of structural abnormalities such as cleft palate, and velopharyngeal insufficiency (hypernasality) or nasal polyps and enlarged adenoids (hyponasality). Assess the student’s resonance looking for difficulties such as hyponasality, hypernasality, nasal emissions, and/or assimilation nasality on vowels.
- Additional Areas of Assessment for Planning Intervention - breath rate, phonatory efficiency, muscle tension, intelligibility, speech avoidance, and s/z ratio and maximum phonation time
The following resources are available for a comprehensive voice evaluation:
- Voice Input Forms
- Oral Peripheral Mechanism Exam
- CAPE-V Procedures and Form
- Voice Related Quality of Life (V-RQOL)
The Voice Severity Rating Scale can be completed after assessment pieces are finished, which provides the SLP with a rubric to assist in determining if a student meets eligibility for voice impairment. Examples of adverse impact may include the following:
- limited participation in the classroom (decreased confidence, refusal to read aloud, decreased questions)
- has difficulty communicating in loud school environments (bus, playground, cafeteria)
- student is demonstrating frustration and/or embarrassment regarding their voice
Consideration of Cultural/Linguistic Differences - It is important to investigate cultural and linguistic variables that may affect voice production. Cultural variations can influence variations in volume, pitch, and quality.
Consideration of Temporary Physical Factors - Voice difficulties as a result of temporary physical factors should not be considered as a voice impairment/disability. These might include factors such as allergies, sinusitis, gastroesophageal reflux, colds, abnormal tonsils or adenoids.
Exit Considerations
For a student that qualifies for SLI due to a voice disorder, they may be exited if their voice disorder has been resolved or if their voice disorder no longer has an adverse impact in the educational setting. For additional information please reference the Considerations when Discussing Discontinuation.
Linguistic Diversity and Multilingual Learners
Overview
To help prevent over-representation of racial and/or ethnic groups within specialized instruction, SLPs and school teams should ensure that their structures, policies, and routines account for language diversity and cultural differences. The term language diversity describes the wide variation in communication form, content and use. For example, variations in vocabulary, morphology, syntax, and phonology may be noted in individuals who communicate in English using regional dialects. Students who are identified as multilingual learners may exhibit communication differences because of language differences, accents or cultural variations. Students who use a dialect of English other than Standard American English are called bidialectal. For example, students whose family uses African American English or a Southern dialect of English and are expected to use Standard American English in school, are bidialectal.
Evaluation
A student must present a language disorder in both languages to qualify as a person with a speech-language disorder. SLPs should do a variety of assessments/modifications to account for cultural and linguistic diversity. When assessing these students a language and developmental history and caregiver input is essential.
Standardized assessments
- Administration of assessments in the student’s primary native and secondary language if they exist (e.g. CELF-Spanish or GFTA-Spanish). If a bilingual SLP is not available, an interpreter can be used. For more information about the use of interpreters please review the FAQ for this document.
- Accommodations and modifications to standardized assessment procedures may be necessary to gain useful information. Acknowledgement of any non-standardized administration and lack of validity to standard scores should be noted in the evaluation report.
- Standard scores should NOT be reported if a test has been translated. A standardized assessment may be translated to obtain helpful information about communication functioning, but standard scores will not be valid. Please review the FAQ for Linguistic Diversity and Multilingual Learners.
Criterion-referenced assessments, dynamic assessments
- Use of informal assessment can be a less-discriminatory resource to understanding what a student knows and can do. In the evaluation report, it is important to describe tasks, how they were presented, student responses and the reasoning behind conclusions drawn.
- Speech and language samples in both languages may offer more insight and opportunity to observe and analyze communication skills that are used functionally. Samples should be obtained in all languages used, with the aid of an interpreter if needed to analyze morphology, syntax, phonology, and lexical systems. Considering both languages can provide helpful information; clinicians must remember that skills across languages may not have a one-to-one correspondence.
Eligibility
In order to qualify students for services under Federal law (IDEA 2004) and state special education rules, the student’s communication difficulties or differences must not be due to cultural or linguistic differences. Characteristics of second language learning described by Roseberry-McKibbins (2002) include:
- Interference (Transfer) – The first language influences use of English.
- Interlanguage – Changes in language rules as the new language is learned.
- Silent period – Listening to the new language with little output
- Code-switching - Using both English and native language
- Language loss – Decrease use of a first language sometimes results in loss of skills as English is being learned.
Service Delivery
Goals should reflect the areas of weakness that are present in the dominant language, not weaknesses due to limited English proficiency. Teaching English as a second language (or Standard American dialect) is not the role of special education. If a student qualifies for EL services, they may also receive special education support if the IEP Team determines that both are appropriate and necessary in order for the student to access the general education curriculum. When working with multilingual learners, the monolingual SLP can utilize visual supports, work with staff to translate materials or interpret for the student, choose student groups in which student partners can support communication, train paraprofessionals to provide language support and collaborate with English Language teachers/staff.
Assessments for Multilingual Learners
Language and development questionnaire
- Alberta Language and Development Questionnaire (ALDeQ)© [URL)
- The Alberta Language and Development Questionnaire (ALDeQ; Paradis, Emmerzael, & Duncan, 2010) was designed to be a parent-reported measure of the first language development of English language learners that is not specific to a particular language/cultural group. This instrument was developed in consultation with the Multicultural Health Brokers Cooperative (http://www.mchb.org), with many questions being based on those from the questionnaire presented in Restrepo (1998). The resulting 18-item ALDeQ was evaluated in a sample of typically developing (TD) children and children with language impairment (LI) with 18 months of exposure to English through preschool or school on average. Validity results were reported for these items. As for limitations, the authors noted that parents of the children with LI knew their children were seeing speech-language pathologists and/or in special kindergarten programs, which could have influenced their responses. (PsycTests Database Record - 2022 APA)
- Family Socio-Cultural Interview (PDF)
Common Standardized Assessments for use with students whose primary language is:
- Spanish
- Comprehensive Language: Preschool Language Scale-5th ed. Spanish (PLS-5 Span.) (Birth-7-11)
- CELF Preschool-2, Spanish (CELF-P-2:S) (3:0-6:11)
- CELF-4, Spanish (CELF-4:S) (5:0-21:11)
- Bilingual English-Spanish Assessment (BESA) (4:0-6:11)
- Syntax: Spanish Structured Photographic expressive Language Test 3 (Spanish SPELT-3) (4:0-9:11)
- Articulation: Goldman-Fristoe Test of Articulation-3rd ed. Spanish (GFTA-3 Span.) (2:0-21:11)
- Arabic
- The Arabic Language: Assessment of Function
- African American Vernacular English
- Diagnostic Evaluation of Language Variation (DELV)
Additional Resources
Alberta Language and Development Questionnaire (ALDeQ)©
Alberta Language and Development Questionnaire (APA PsychNet)
Family Socio-Cultural Interview (Google Doc)
Low Incidence Populations
Overview
The purpose of this document is to discuss the SLP's role in working with students with low incidence disabilities. Students with the primary eligibility of cognitive impairment, severe multiple impairment (SXI), physical or otherwise health impaired (POHI), Deaf and hard of hearing (DHH), visual impairment (VI) or autism spectrum disorder (ASD) may require categorical special education programs. Many of these students may have various levels of complex communication needs (CCN) which the SLP, in partnership with the classroom teacher, may address.
Evaluation
ASD Evaluation
- According to MARSE, the multidisciplinary evaluation team for ASD eligibility must include a school psychologist or psychiatrist, school social worker, and SLP. The ISD or LEA can choose to include others, such as the occupational therapist (OT) or teacher consultant (TC), but they are not required.
- It is strongly recommended that an ASD evaluation should be based heavily on observational data completed by all multi-disciplinary team members across both academic and nonacademic settings. Consider observing the student prior to completing checklists or standardized rating scales by using the Evaluation Team Observation Form & Probe Questions. The Education-Based Evaluations for Autism Spectrum Disorder document provides examples of specific interactions and quotes from the observation and should be utilized when gathering evidence for and evidence against in the social, communication, and behavioral domains. MARSE Eligibility Observation Form for ASD.
SXI Evaluation
- Due to many sensory and physical limitations, students in severely-multiply impaired programs may have difficulty completing standardized tests. Speech and language testing for students with this eligibility should involve informal assessments (Communication Matrix, The Interactive LCPS Continuum Of Language Expression (Google Sheets), etc). caregiver/teacher interviews, developmental history, and observations in addition to any appropriate formal testing that can be completed.
Service Delivery
Speech-language as a related service should be considered based on the complexity of the student's current needs and expected developmental milestones. When determining what services are necessary for the IEP, the student’s age and grade should be taken into consideration due to the importance of early intervention. Direct services should be utilized for preschool and early elementary with consultation and push-in services prioritized for upper elementary and beyond if the student's needs are able to be met by supports and services of the center-based program.
Goals should be identified that have the most adverse impact within the school environment. This includes social opportunities that can be found in unstructured settings such as recess, electives, lunch, transitions between classes etc. The overall goal when working with all students should be to ensure that the student has functional communication skills and is an autonomous communicator. In supporting students identified with an Autism Spectrum Disorder, shared goals for pragmatics with the SLP, social worker and occupational therapist and/or the special education teacher should be strongly considered and in support of the Least Restrictive Environment. When multiple providers are working together on identified and specific goals that support the students’ lagging skills, the opportunity for generalization can be realized.
Exit Considerations
It is important to note, if the student’s speech-language needs are being met through specialized instruction provided by the special educator, then the SLP is not required to continue services on the IEP. Supporting data must be quantified with multiple data points within the PLAAFP demonstrating that the student does not need specialized instruction provided by the SLP and that the student’s speech-language needs are being met through another service/program. Therefore, direct or consultative services may not be warranted and the student can be moved to a consultative service delivery if needed or no services.
Additional Resources
Evaluation Team Observation Form & Probe Questions
The Education-Based Evaluations for Autism Spectrum Disorder
MARSE Eligibility Observation Form for ASD
Communication Matrix
The Interactive LCPS Continuum Of Language Expression
Augmentative and Alternative Communication (AAC)
Overview
Communication is necessary for social connectedness and is the essence of human life. This belief creates a unique lens when implementing systems and supports for Augmentative and Alternative Communication (AAC) due to the nature and role of communication in learning and life. AAC, as defined by ASHA, is an area of practice that supplements or compensates for impairments in speech-language production and/or comprehension. AAC describes the multiple ways a person can communicate that could supplement or replace their spoken language. AAC is truly multimodal and incorporates the individual’s full communication abilities which may include any existing speech/vocalizations, gestures, manual signs and/or aided communication. AAC devices supports and services fall under the category of Assistive Technology (AT). Under IDEA/MARSE, AT must be considered for each student receiving special education services, regardless of age or disability. The SLP should be leading and/or participating in this process as a vital member of the IEP team.
Evaluation & Eligibility
Wayne RESA, consistent with ASHA, advocates and strongly agrees that communication pervades all aspects of education. Subsequently, there are no prerequisites to begin use of AAC supports. This means that there are no required cognitive skills, physical abilities, behavioral skills, minimum age, or communicative intent needed to begin use of AAC supports. AAC should be considered for individuals who have some speech or speech that is unintelligible to unfamiliar listeners, in addition to non-speaking students. AAC does not delay or prevent acquisition of verbal speech and language development.
The decision to introduce AAC should be made as a team including the family, SLP, and other professionals from the IEP team. That being said, no individual should go without communication and all students should have access to AAC that promotes effective communication. In Wayne County, a version of a core vocabulary board (PDF) has been developed and made available as a universal communication support to use with students. A core vocabulary board on its own will not provide a student with access to becoming an autonomous communicator. The goal of using AAC is to ensure that an individual will become an autonomous communicator, meaning that they can say whatever it is they want to say, whenever they want to say it, with whomever they want to say it to.
Choosing an aided AAC system requires a team based consideration of the student’s current skills, strengths and needs; while remembering to not restrict the student’s potential. There is not a one-size-fits-all equipment recommendation for any age or developmental level. Assessment and consideration should be reflected through the SETT framework. SETT is an acronym for Student, Environment, Tasks and Tools. The SETT framework, developed by Joy Zabala, can be used to guide collaborative decisions about devices and services. AAC assessments should be a collaborative, dynamic, on-going process that happens while the student is actively learning and is reconsidered each year even after an AAC system has been selected. AAC assessment can lead to a better understanding of the student’s preference for different symbol sets, access methods, language organization, environments and communication partner support needed.
Service Delivery
AAC therapy is an essential language therapy, therefore consider the basic principles of language therapy and functional communication skills when establishing goals. The best way to learn AAC and language is during engaging daily communication activities and interactions in the natural environment. All communication partners must be trained to demonstrate augmented input (otherwise known as “aided language stimulation” or “modeling”) to support and increase symbol comprehension and expressive production.
Both direct and consultative services may be needed to support a student who uses AAC. Examples of consultation may include but are not limited to: engineering the environment to increase opportunities for communication, programming and maintaining AAC systems, and training teachers/staff/family on AAC use across environments.
Exit Considerations
Dismissal from services must be considered on a case by case basis in order to meet the individual needs of each student and not based on age and/or programming. Before dismissing from services, ensure the student can participate fully in communication interactions and has achieved the fundamental rights outlined in the Communication Bill of Rights. Additionally, prior to dismissal from services, ensure there is a plan in place to address system repairs/replacements, training new communication partners and workplace needs.
Additional Resources
Vocabulary Board
SETT Framework - Joy Zabala, Ed.D. Creator of the SETT Framework
SETT Framework
Communication Bill of Rights
Early Childhood Speech & Language Overview
Overview
Early intervention is a system of services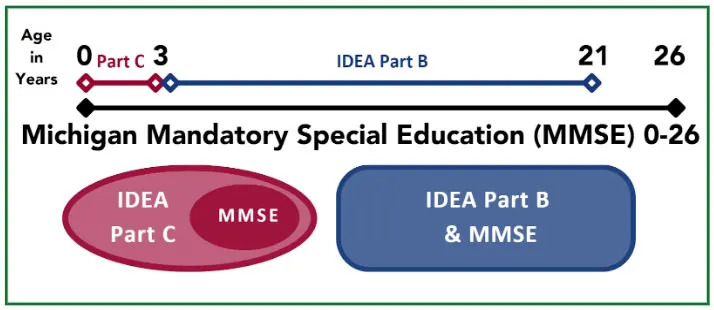 that helps infants, toddlers and preschoolers with developmental delays or disabilities. Early intervention focuses on helping eligible infants and toddlers learn the basic and brand-new skills that typically develop during the first three years of life, such as: Physical, cognitive, communication, social/emotional, and self-help skills. The Individuals with Disabilities Education Act (IDEA) requires services to infants and toddlers under Part C of the act, and services to children ages 3-5 years are required by Part B of the act.
that helps infants, toddlers and preschoolers with developmental delays or disabilities. Early intervention focuses on helping eligible infants and toddlers learn the basic and brand-new skills that typically develop during the first three years of life, such as: Physical, cognitive, communication, social/emotional, and self-help skills. The Individuals with Disabilities Education Act (IDEA) requires services to infants and toddlers under Part C of the act, and services to children ages 3-5 years are required by Part B of the act.
The purpose of Early Intervention is to enable young children (birth to 5) to be active and successful participants during the early childhood years and in the future in a variety of settings – in their homes, with their families, in childcare, in preschool, and in the community. Most referrals to Early Intervention received in Wayne County are due to speech concerns. The SLP may play a critical role in these services. The SLP may be the primary service provider (PSP) or support the PSP depending on the service delivery model.
Definitions
- Part B: Early Childhood Special Education 3-5 years
- Part C: Early On - Birth to 3
- Primary Service Provider (PSP): One member of the team functioning as the primary connection between the family and other team members.
Evaluation & Eligibility
Evaluation for Early On eligibility can be met when an infant or toddler exhibits 20% delay in any area of development or has an established condition that is known to cause a delay. Early On Michigan Mandatory Special Education (Part C) can be met when an infant or toddler meets one of the MARSE eligibility criteria. Early Childhood Special Education (Part B) eligibility is met when a child is evaluated and meets one of the MARSE eligibility criteria.
Child Outcomes
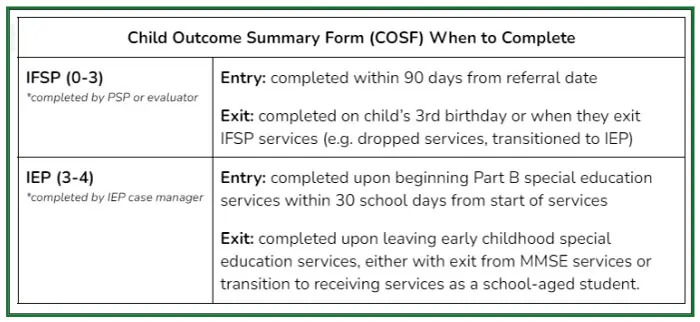 Child Outcome Summary process synthesizes information on a child’s progress and functioning across settings and is required to be reported at entry and exit of Early On and preschool special education services. The document collects, analyzes and uses this data to measure progress towards results, improving services and for additional federal reporting purposes. The IFSP/IEP Team is responsible for summarizing information about the child’s functioning from multiple sources but must include a tool that assesses all developmental domains (e.g. Brigance, Carolina Curriculum, MEISR). The Early On Training and Technical Assistance website provides everything to know for child outcomes training and resources.
Child Outcome Summary process synthesizes information on a child’s progress and functioning across settings and is required to be reported at entry and exit of Early On and preschool special education services. The document collects, analyzes and uses this data to measure progress towards results, improving services and for additional federal reporting purposes. The IFSP/IEP Team is responsible for summarizing information about the child’s functioning from multiple sources but must include a tool that assesses all developmental domains (e.g. Brigance, Carolina Curriculum, MEISR). The Early On Training and Technical Assistance website provides everything to know for child outcomes training and resources.
Service Delivery And Family Involvement
Early On services may be provided by the primary service provider (PSP) who could include other service providers as needs are identified. Early Childhood services may be provided by an education team as outlined in the child’s IEP. However, it is important to note that parents play an essential role in the evaluation, assessment, determination of outcomes, planning, service delivery and transition for their child(ren) during their time in Early Intervention. Family support and engagement are crucial to achieving the desired child and family outcomes. Services are offered within the child’s natural environment (home, community and/or other settings; individually or within a group as listed on the child’s IFSP/IEP. Services are offered year round for Early On. Services for 3-5 year olds may align with a school district’s calendar.
Early OnⓇ - Birth to 3 years old (IDEA PART C)
Early OnⓇ is described as services provided to children ages birth to 3 years of age (0-36 months) who are at risk for developmental delays and/or disabilities. While the IDEA regulations include special education services for children ages 3-21, Michigan Mandatory Special Education (MMSE) extends this range from birth-26. In Michigan, the State Department of Education has been designated as the lead agency for coordination among school and non-school agencies for services for children ages birth through 3 years old through Early On referrals received then divided up to evaluation teams. If found eligible, an Individualized Family Service Plan (IFSP) should be developed within 45 calendar days of receiving the referral.
Evaluation
Best practice warrants a play-based evaluation completed within a natural environment. To determine eligibility, informed clinical opinion should be derived from multiple sources of information.
- Team: The child developmental assessment is completed by the child’s caregiver along with two evaluators from two different disciplines (teacher, SLP, SSW, PT, OT, psychologist and/or school nurse).
- Adjusting for prematurity is needed for every child born at 36 weeks gestation or earlier. This adjustment should continue until the child reaches the chronological age of 24 months.
- Types of Information Needed:
- Hearing and Vision Screening
- Medical Documents: request a health appraisal from the child’s doctor(s)
- Routines-based Assessments and informal observations
- Observation of Parent/Child Interaction
- Developmental History
- Evaluation on All Areas of Development - adaptive, cognition, communication, motor and social emotional
- Additional Factors to Consider During Birth-3 Evaluations can be found in the FAQ.
Eligibility
It is important to consider the functional impact (vs. educational) of the child’s delay(s)/disability on their development. There should be documented evidence of adverse impact on the child’s participation in age appropriate activities (including daily routines, play and interactions with others). The suspected disability cannot be due to limited English proficiency. Eligibility determination is based on an analysis of comprehensive data from a variety of sources including two evaluators of different disciplines, the standardized child evaluation, parent/caregiver interview, developmental and medical history, observation of the parent/child and the functional routines assessment of the child/family. Refer to: Evaluation and Eligibility (ccresa.org).
According to the Michigan Part C State Plan, adjusting for prematurity is needed for every child born earlier than 37 weeks gestation. This adjustment should continue until the child reaches the chronological age of 24 months. After the child is two years old (chronologically), adjustments for prematurity will be discontinued. Ex: Child born at 36 weeks, chronological age is 18 months, evaluation and assessment scores show the child functioning at 17 months – with the adjusted age there is no delay.
Early On Eligibility:
- When a referral is received for a child with an established condition, it is not required to administer an evaluation tool. Please see the Early On Established Conditions List updated 11-3-21 (ccresa.org). The team must continue the information gathering process consistent with any other referral outlined above under evaluation.
- Developmental Delay under 2 months old (adjusted age) any delay, 2 months – 36 months old a delay of 20% or 1 standard deviation below the mean in one or more developmental domains.
Note: Using informed clinical opinion - Early On uses informed clinical opinion, in addition to the documented evidence, when recommending initial eligibility for services under Early On. Informed clinical opinion makes use of qualitative and quantitative information to assist in forming a determination regarding difficult to measure aspects of current developmental status and the potential need for early intervention. In order for a provider to use informed clinical opinion, he or she must have appropriate training, previous experience with evaluation and assessment, sensitivity to cultural needs, and the ability to elicit and include family perceptions (Lucas and Shaw, 2012). Informed clinical opinion may not be used to negate the results of evaluation instruments used to establish eligibility.
Michigan Mandatory Special Education Eligibility - Michigan Administrative Rules for Special Education (MARSE) With Related IDEA Federal Regulations.
Additional Factors to Consider When Evaluating:
A variety of factors can be predictive of later language outcomes. The child’s functions, means, and frequency of communication, rate of vocabulary growth including use of verbs, comprehension skills, and early sound development should be considered. The following areas should also be considered when evaluating a child:
- medical and developmental history
- hearing
- motor and cognitive skills
- imitative skills
- emotional and social functioning
- feeding and swallowing
- oral motor system
- play skills
- emergent literacy
- environmental stressors
- parent/guardian-child interactions
- level of caregiver concern
A variety of factors can be predictive of later language outcomes. The child’s functions, means, and frequency of communication, rate of vocabulary growth including use of verbs, comprehension skills, and early sound development should be considered.
Preschool Special Education: 3 to 5 years (Part B)
IDEA Part B qualifies children and youth ages 3 through 21 years old to receive special education and related services, ensuring a free and appropriate public education in the least restrictive environment. A referral can be made by anyone on behalf of the child, however the legal caregiver (e.g. parent, foster parent, etc.) is required to consent to the evaluation. Intake staff/Special education office (e.g. through Child Find) should gather information related to developmental concerns through a caregiver interview upon scheduling.
Part B services may start when a child turns 2 years and 6 months old:
- If the child has been receiving services with an IFSP, under Part C, then a transition plan and conference must take place between the ages of 2 years 3 months and 2 years 9 months, to support transition to the IEP.
- OR If the child is identified after age 3, an IEP needs to be completed within 30 school days from the start of referral.
Evaluation
Best practice warrants a play-based evaluation completed within a natural environment including parent/caregiver participation. With the child being preschool age please reference the guidance provided on Speech and language evaluations and eligibility. An all domain assessment tool, such as the Battelle Screener, along with observation, parent input, and an interview to obtain information about the child's skills in daily activities, routines across settings should be completed in order to determine eligibility and report Child Outcome Summary data (COS).
Eligibility
While preschool is not required in the state of Michigan, a preschool-aged child (3-5 years old) has access to IDEA Part B Special Education Services. The child may receive an evaluation to determine eligibility as part of the Part C or Part B transition or through the Child Find process. An appropriate evaluation is non-discriminatory, uses sound materials and procedures, and is administered in all areas of disability by qualified staff. Based on consideration of all required information, a group including the parent and other qualified individuals determines whether the child is eligible under MARSE. There should be documented evidence of adverse impact on the child’s participation in age-appropriate activities (including daily routines, play and interactions with others) as well as educational impact. The suspected disability cannot be due to limited English proficiency. Eligibility determination is based on the analysis of comprehensive data, and must not be from any single measure or assessment. The child must be assessed in all areas related to the suspected disability, including, if appropriate, health, vision, hearing, social and emotional status, general intelligence, academic performance, communicative status, and motor abilities.
Transition Planning
For children who have received Early Childhood special education services may transition to preschool or other educational settings. It is important that active participation from the primary service provider (PSP), families, preschool staff and other relevant professionals occurs during this transition planning to ensure a smooth transition and continuity of services.
Exit Considerations
Before exiting the Early Childhood program, it is important to conduct a comprehensive evaluation to assess the child’s current communication and language skills. This evaluation should include a review of progress reports, assessments, and observations to determine if the child has achieved their goals and if further speech-language services are necessary. It is important that all relevant records, including assessments, progress reports and current IEP are transferred to the receiving program or school district. This enables the new team to have a comprehensive understanding of the child’s needs, progress and recommended supports.
FAQ: Caseload / Workload Service Delivery
| Direct | Consult |
|---|---|
Provider works directly with the student. | Provider observes, informally assesses, or works with the student. |
Work with the student is related directly to the goals and objectives (may be collaborative with another provider). | Provider consults with the teacher and/or parent/guardian; discussion and activities are related to goals and objectives that the teacher and related service provider are working on with the student |
Progress reports are completed by the related service provider. | Progress reports are completed collaboratively by both the teacher and the related service provider. |
Provider documents service provisions. | Provider documents service provision and consultation activities. |
The student is counted on the provider’s caseload. | The student is counted on the provider’s caseload. |
- How do the roles and responsibilities of the various levels of service compare?
See table above. - How do I document direct/consultative services in the IEP?
Direct and/or consultative services should be documented separately and include the total time and frequency that each service will be provided. - Do I need to complete a REED if adding/dismissing speech-language as a related service?
If the student has met their IEP goals and objectives and it is determined that there are no other identified speech-language areas of need, then speech-language as a related service can be dismissed without completing a REED. Instead, you may use the progress monitoring data to provide information needed in the PLAAFP to dismiss the service. However, if you are collecting data through a formal process (assessment, observation, etc.) to determine the need for related services, then a REED is required for determining a need for service or to exit the service and for parent/guardian notice. IDEA states that if the IEP Team and other qualified professionals, as appropriate, determine no additional data is needed to determine whether the student continues to be a student with a disability/determine educational needs, the district must notify the parent/guardian the reason that no additional data is needed. In that case, the parent/guardians have a right to request an assessment to determine whether the student continues to be a student with a disability, and to determine the student’s educational needs. - What might a caseload look like that abides by MARSE rules with a caseload size based “upon the severity and multiplicity of disabilities, allowing time for diagnostics, report writing, consulting with parents/teachers, IEP meetings and travel between buildings (MARSE)?”
Completing ASHA’s Workload Calculator is the first step to determine an appropriate caseload size that considers these factors, including those beyond MARSE such as Service Capture/Medicaid Billing, monitor services, and MTSS/RtI. Special consideration should be given to caseloads that service self-contained programs, have additional evaluation responsibilities, and require travel between multiple buildings. - Do initial evaluations count toward caseloads?
Yes, MARSE specifically states that evaluations “shall be counted as part of the caseload.” Any student being evaluated will count toward the caseload cap outlined in this rule. One evaluation is equivalent to one caseload student. This also applies to SLPs with assignments to complete evaluations above and beyond the initial/re-evaluation requirements for their building(s) assignment (e.g. Early Childhood Evaluations via Child Find, a Diagnostic Evaluation Team (ASD), etc.). For example, if a SLP is evaluating 3 students/month, then the caseload should reflect that number. - What should a caseload look like for a SLP providing birth-3 services?
Caseload considerations vary when comparing SLP services as a primary service provider (PSP) within Part C birth-3 programming vs. Part B school-based SLP services. Some considerations include 1)PSP/transdisciplinary approach with parent/caregiver coaching within sessions, 2) frequency and length of visits (45-60 minutes), 3) Parent/caregiver education (individually or within group settings), 4) travel time, 5) completing Part C to Part B transitions, 6) weekly evaluation(s), 7) completing speech-language evaluations/updates for personal and team caseloads and 8) providing consultations for team members, 9) bi-annual review of IFSP, 10) Service capture documentation. - How would an IEP Team determine who assures implementation of the IEP (Designated Case Manager)?
The IEP Team must consider relevant factors in making this decision including: eligibility, nature of disability, service time and staffing considerations (time provider is in student’s building). Most often the staff with the highest level of contact with the student assumes this role, however this should not always be the primary determination. For example, the SLP may have the most frequent IEP minutes with the student, however due to the nature of their disability (behavior, physical needs, etc.) another staff member may be more appropriate to ensure IEP implementation. How should monitoring be counted?
It is Kent ISD’s guidance that monitoring should be used cautiously unless it has been determined that it supports a measurable outcome for the student in the least restrictive environment. When this occurs, a workload approach is recommended.
FAQ: Evaluation / Eligibility Overview
- If a SLP participates in a multidisciplinary evaluation with other staff in which other eligibility areas are being considered (e.g. CI, ASD, SLD, etc.), does the team need to consider SLI as an additional eligibility area on the Eligibility Report? If a SLP came into the process as a multidisciplinary team member and SLI is not the primary concern, the Eligibility Report does not have to reflect that SLI was considered. However, in the REED document, you must check the box that states “Appropriate programs or services in special education” in the “Purpose” section.
- How are outside evaluations incorporated in a school evaluation? Information from outside reports, such as standardized assessment data, should be reviewed and considered as part of the evaluation process. This data should be included as part of the REED and/or Eligibility Recommendation. When outside evaluation information is provided to a district outside of an evaluation cycle, the IEP Team should demonstrate consideration of the results by reflecting the information within the IEP or through Prior Written Notice by initiating a REED (if needed).
- What level of absenteeism or lack of exposure to the curriculum disqualifies a student for eligibility? When considering speech and language concerns, the level of absenteeism or lack of exposure to the curriculum does not discount a student for eligibility as the evaluation/IEP team should be looking at the whole student and not just a period of time.
- Should age or grade equivalent scores be used in making eligibility decisions? No. Neither should be used, equivalents do not account for normal variation around the test mean and the scale is not an equal interval scale. Therefore, the significance of delay at different ages is not the same. Furthermore, differing ages of students within the same grade make comparisons between students within and between grades difficult. In addition, grade equivalents do not relate to the curriculum content at that level. While seemingly easy to understand, equivalent scores are highly subject to misinterpretation and should not be used to determine whether a student has a significant deficit.
- Can you modify standardized test procedures? Modifications of standardized test procedures invalidate the use of test norms, but may provide qualitative information about the student’s language abilities. If test administration appears to be invalid for any reason, test scores should not be subjected to usual interpretations and the reasons for invalidation should be clearly stated in oral and written presentations of test results as explicitly addressed in federal regulations.
- Can one-word vocabulary tests be used in the assessment process to qualify students for speech and language services? They should be used with caution as studies have found that single word vocabulary tests have poor psychometric properties and/or are not representative of linguistic competence embedded in life activities.
- Who can sign as a parent/guardian on a REED? MARSE states that “Parent” means any of the following: (i) A biological or adoptive parent of a child. (ii) A foster parent, unless state law, regulations, or contractual obligations with a state or local entity prohibit a foster parent from acting as a parent. (iii) A guardian generally authorized to act as the child’s parent, or authorized to make educational decisions for the child, but not the state if the child is a ward of the state. (iv) An individual acting in the place of a biological or adoptive parent, including a grandparent, stepparent, or other relative, with whom the child lives, or an individual who is legally responsible for the child’s welfare. (v) A surrogate parent who has been appointed can be utilized if the student is a ward of the state and not residing with the student’s parent(s). After reasonable efforts have been made to contact the parent in the case of a ward of the state, a surrogate parent will need to be identified to provide consent.
- What if a parent/guardian refuses to sign consent for an initial evaluation through the REED process? If a parent/guardian refuses consent, the district may not proceed with the evaluation. If the district disagrees with a parent/guardian’s refusal, the IEP Team should contact the Director of Special Education to discuss potential options for next steps.
- What if a parent/guardian/student requests that services are discontinued when a student is still eligible? The parent/guardian/student (age of majority) would sign a Revocation and Notice of Cessation to discontinue services. Notification to your Special Education Administrator should be considered or followed per local process and procedures.
FAQ: Speech Sound Disorders
What do you do when a student is not making progress? It is expected various methods and strategies be employed and documented prior to service level reduction. Tracking the student’s response to the intervention provided, followed by attempts to use different approaches to intervention should be considered when making decisions to remove services. When the student has plateaued in their progress and multiple attempts have been made to redesign services, the team may discuss whether there is a lack of educational benefit. The team should make decisions about how to proceed with the input of district administrators. Refer to MSHA, 2006 SLRS-4 for more information.
Do you consider developmental norms when treating lateralization? Lateralization of /s, z, sh, ch, j/ does not undergo spontaneous improvement with age, and therefore, should not be considered developmental. In determination of eligibility, further investigation is warranted regarding stimulability and prognosis for treatment, response to early intervening, and adverse educational effect.
- What about students with single sound errors? When single sound errors are identified, the adverse educational effect should be considered very seriously. Students who have one sound in error often experience difficulty in the classroom with social relationships, literacy skills, and vocational outcomes. In these cases, early intervention, provided either directly or indirectly with the help of parents/guardians and/or teachers, may result in improved articulation. Some districts have reported success in reducing the number of articulation referrals for students with 1-2 sound errors by providing short term intervention. It is imperative to support their educational needs by intervening when necessary, regardless of the number of speech sounds in error.
- Does dentition or tongue thrust impact speech sound production? Yes. Dentition and tongue movements should be evaluated with an oral peripheral exam, which can impact articulation and intervention. Students who have differences in dentition or tongue thrust must have a speech disorder that adversely affects school performance to be considered eligible for articulation services. See Oral Peripheral Mechanism Examination.
When should you consider using an augmentative/alternative communication system? When a student is making slow progress in treatment, and there is a significant impact on academic and social communication due to poor speech intelligibility, strong consideration should be given to use of augmentative/alternative systems (AAC). Refer to the Augmentative and Alternative Communication accordion above.
Do students with a history of cleft lip/palate respond to speech therapy? Approaches to treatment for articulation disorders associated with cleft palate or velopharyngeal dysfunction (VPD) will depend on whether or not speech deviations are obligatory (e.g. related to atypical anatomy and/or structural defects) or learned.
Obligatory speech deviations that are related to true VPD or other structural deviations such as fistulas are not responsive to speech therapy and will likely require surgical intervention or other physical management.
Learned articulation errors (e.g. compensatory errors and phoneme-specific nasal air emission) should be responsive to speech therapy.
Do you need two standardized scores to qualify a student for an articulation impairment? You do not need to complete two standardized assessments to qualify a student SLI in the area of articulation. You should use at least two different evaluation tools to support your eligibility, which may include a standardized score, observations, student/teacher/parent input, or analyzing a speech sample for intelligibility or PCC.
If a student has a phonological processing disorder, would it fall under the sub area of articulation or language? Based on ASHA's updated definition of speech sound disorders as an umbrella term for errors in articulation and phonology, it is Wayne RESA’s recommendation to use the sub area of articulation for all impairments in speech sound disorders where this is the primary impairment.
FAQ: Language
- How do you distinguish a language impairment from a language difference?“No” answers may indicate impairment, while “Yes” answers typically indicate English language learning. Refer to Section Seven: ELL for more information. When considering whether a student presents with a language impairment rather than typical differences of English Language Learners, two questions to ask are:
- Does the student present with average language skills in their home language?
- Is the student learning English at a similar rate than comparable peers?
- How do you distinguish a language impairment from an attention difficulty? While attention difficulties can in many ways present similarly to a receptive language difficulty, one way to help differentiate is whether strategies like repetition and active listening significantly improve the student’s comprehension. An example of this is giving a verbal direction to a student. If the student does not respond correctly at first, teach them to use active listening (eyes on the speaker, body calm, etc.) and then repeat the direction. If they are able to respond correctly this time, this may indicate that the difficulty was attention rather than a language impairment. If they still do not respond correctly, even with repetition and active listening, this may indicate that they did not understand the direction, which could be related to a language difficulty.
- How do you distinguish a language impairment from a behavior difficulty? Similar to differentiating a language impairment from an attention difficulty, it is important to investigate if the student is able to exhibit a skill at all or under certain circumstances. For example, if a student does not respond to a direction unless given an incentive, this indicates that the student understood the direction but chose when to respond. If the student does not exhibit the skill despite motivation or incentive, this indicates that they do not have the skill, which could indicate a language difficulty versus a choice, or behavior. Consult with other evaluation team members if another eligibility is suspected.
- How do you effectively evaluate pragmatic language? Pragmatics involves three major language skills (communicative intent/engagement, nonverbal rules of conversation, and verbal rules of conversation) which must be addressed during an evaluation. In assessing the pragmatic skills of students, it is important for an SLP to address both developmental expectations and the functional efficiency of the interaction. As a result, the SLP must rely on developmental checklists and observation of students in various environments throughout the school setting and with various communicative interactions with others. With careful observation, parent and teacher report, and appropriate pragmatic language rating skills a reliable eligibility recommendation can be made.
- What is meant by Dynamic Assessment? Dynamic assessment is a method of conducting a language assessment which seeks to identify the skills that the student possesses as well as their learning potential. This enables the examiner to determine what type and degree of assistance the student requires in order to be successful. Dynamic assessment is a fluid evaluation process that identifies the skills a student possesses, how a student is learning, and their potential for learning. In comparison, a static model of assessment (e.g. standardized test) identifies knowledge previously learned. Dynamic assessment requires active participation and uses a test-teach-retest method to evaluate a student’s responsiveness to instruction. It can also help differentiate students with a language difference from students with a language impairment, especially for students from culturally and linguistically diverse backgrounds. Students who are able to make significant changes in short term teaching sessions likely have a language difference but students who are unable to make these changes likely have a language impairment.
- What is a Social Communication Disorder? Per ASHA “Children with language disorders may also present with social communication difficulties characterized by persistent difficulties with the use of verbal and nonverbal language for social purposes. More information about social communication can be found on ASHA’s Social Communication Disorder Practice Portal site.”
FAQ: Fluency
- How do you differentiate between typical speech disfluencies and stuttering? Stuttering usually starts between 2 and 6 years of age. Many students go through periods of disfluency lasting less than 6 months. Stuttering lasting longer than this may need treatment. ASHA Practice Portal for Childhood Fluency Disorders states: “All speakers produce disfluencies, which may include hesitations, such as silent pauses, and interjections of word fillers (e.g. "The color is like red") and nonword fillers (e.g. "The color is uh red"). Other examples include whole-word repetitions (e.g. "But-but I don't want to go") and phrase repetitions or revisions (e.g. "This is a- this is a problem"). These are generally considered to be non-stuttered (typical) disfluencies. When a student uses a high number of non-stuttered (typical) disfluencies, differential diagnosis is critical to distinguish between stuttering, avoidance, and a language disorder.” Stuttering-like disfluencies include part-word or sound or syllable repetitions, prolongations, and blocks which are usually accompanied by extra effort or tension.
- How do you distinguish cluttering from stuttering? Signs and symptoms of cluttering include: rapid and/or irregular speech rate, excessive coarticulation resulting in the collapsing and/or deletion of syllables and/or word endings, excessive disfluencies, which are usually of the more non-stuttering type (e.g. excessive revisions and/or use of filler words, such as "um"), pauses in places typically not expected syntactically, unusual prosody. Students who stutter are more likely to be self-aware. For detailed information regarding cluttering, please see: Fluency Disorders: Signs and Symptoms on the ASHA website.
Differential diagnosis of stuttering vs. cluttering can be difficult. The following characteristics are essential in diagnosing cluttering: excessive number of whole-word or phrase repetitions, poorly organized thinking, short attention span and poor concentration, and lack of complete awareness of the problem (Daly, 1996). Since thought organization is one the most apparent symptoms displayed by the student, a thorough language evaluation, including written expression, is necessary if cluttering is suspected.
- What are the Risk Factors associated with stuttering?
Risk Factor Elevated Risk Gender/Sex Male (stuttering affects males 3-4x more than females) Family history Family history of stuttering (especially persistent stuttering) Age of onset Children who begin stuttering before age 3½ years are more likely to outgrow it Total time since onset If it has been more than 6-12 months or no improvement in stuttering over several months, a person is more likely to have persistent stuttering Pattern of stuttering Presence of prolongations or blocks and secondary behaviors increase likelihood of stuttering. (whole word repetitions at the beginning of utterances are more typical in development than stuttering blocks) Awareness If the student is relatively unaware of their disfluencies, the risk for a fluency disorder is reduced compared to a student who is aware of their stuttering. Poor articulation or phonological skills Presence of their speech-language impairment increases the risk of fluency disorders Environment Family reaction, fast-paced family schedule, family dynamics such as high expectations, communication style of parents/guardians and/or teachers, significant life event (death, divorce, etc.) Sensitivity of student A student who is more emotionally sensitive may respond to stressful situations with stuttering behaviors.
- What are some of the exit considerations specific to fluency disorders and what about a 504 plan?A 504 plan should be considered when a student no longer meets eligibility criteria (e.g. may continue to stutter but no longer requires specialized instruction), they may be eligible for a 504 plan. A 504 plan covers a disability that substantially limits one or more major life activities. With regards to fluency disorders, 504 accommodations may include:
- using audio/video recording for oral presentations,
- increasing the time provided for an oral reading or presentation,
- providing an alternative assignment to oral reading,
- altering the size of the group or audience for presentations
- student given opportunities to ask questions to the teacher in private
- What about atypical disfluencies and how does traditional fluency intervention work for students? Atypical Disfluency is a speech disorder that seems related to stuttering. The last syllable or sound of a word is repeated. The disfluency is similar to stuttering, only with the broken sounds and syllables coming at the ends of words instead of the typical beginning (e.g. final part-word repetition, mid-word insertion of breath, broken words, and final sound prolongation). Atypical disfluency is not especially responsive to traditional fluency intervention.
The SLP must consider the degree to which the individual’s disfluent behaviors and overall communication are influenced by a coexisting disorder (e.g. other speech or language disorders, Down Syndrome, Autism Spectrum Disorder, Attention Deficit Hyperactivity Disorder) and determines how treatment might be adjusted accordingly. The SLP should understand the interaction of symptoms and the strategies that are most effective for dealing with stuttering, cluttering, and atypical disfluencies when they occur together. The goal is to help the student understand and manage their disfluency.
- Are there special factors that should be considered for bilingual students who stutter? Yes. Bilingual students who stutter typically do so in both languages. Disfluent bilingual students produce more mazes than their monolingual peers, which can be misdiagnosed as stuttering. Therefore, the presence of audible or inaudible sound prolongations, excess tension, and parent/guardian concern for stuttering must be considered to diagnose stuttering in bilingual students.
FAQ: Linguistic Diversity and Multilingual Learners
- How does the dominant language influence English learning, in terms of disability? Remember, goals should reflect the areas of weakness that are present in the dominant language, not weaknesses due to limited English proficiency. Reference the Language Chart for examples of the influence of different languages on English.
- How does Language 1 influence speech sounds while learning Language 2? Assessment of a student with articulation, fluency, or voice concerns would follow standard procedure for other speech assessments, yet limited English proficiency still needs to be ruled out as a factor. The assessment will need to take place in the student’s native language to determine whether speech needs are present in the native language, culturally acceptable, or identified through case history. See ASHA’s Phonemic Inventories and Cultural and Linguistic Information Across Languages page for specific variations by language.
- Considering there is often a silent period when students learn a new language, when should I evaluate? There is no standard “wait time” for an evaluation. Per Child Find, an evaluation should be conducted when there is a suspicion of disability. However, language differences, acculturation, and efficacy of the language assistance program should all be considered prior to evaluating.
- For students who are new to the country or students who have been adopted and no information exists about previous schooling, how long do I wait to evaluate? If there is a documented disability or established condition (e.g. Down Syndrome, Cleft Palate, Cerebral Palsy), the evaluation team must immediately proceed to an evaluation. In other cases, follow protocol in this section to review whatever educational information exists and performance as compared to peers and progress given language support. This may look different for different students. Remember that limited English proficiency needs to be ruled out in order to consider a special education eligibility but also that a special education evaluation should not be delayed due to English proficiency status.
- What are some 2nd language questionnaires and rating scales and culturally sensitive parent/guardian input forms? See Multilingual Family Input - Socio-Cultural Interview
- When assessing English learners, do I need to utilize the same test in both languages? Because no two tests have a 1:1 correspondence and may assess different grammatical forms, structure, and rely on different cultural background information, using the “same” test in two languages isn’t necessary. The practice of using a standardized English version with an interpreter should be discouraged (e.g. CELF-5 and CELF-4: Spanish). Even if a standardized assessment exists in a student’s native language, cultural differences and normative sample should still be considered when documenting results.
- How do I work with an interpreter/EL staff? When collaborating with interpreters, translators, or EL staff, a SLP remains responsible for planning the session, selecting culturally relevant materials, and appropriately providing service.
- Interpreters should be used to assist the SLP and team throughout the pre-referral and assessment process, unless a speech-language pathologist is fluent in the student’s native language. The person used as an interpreter should be fluent in both oral and written modalities of the languages spoken by the student. The interpreters facilitate communication with the family, participate in gathering background and assessment data, and help communicate assessment results and interpretations during meetings.
- The interpreter must be present during assessment and parent conferences. The role of the interpreter must be defined for the family. Prior to the assessment the SLP should meet with the interpreter and discuss the assessment, including the following:
- Discuss roles and responsibilities during assessment.
- Review key concepts, phrases, words, and procedures that will be used.
- Remind the interpreter that he/she must not alter, omit, or add to the communication.
- Ask the interpreter if specific concepts/words are not translatable.
- Ask the interpreter about cultural considerations for the testing event
- Who is responsible for testing and translation especially with less occurring languages? It is the resident district’s responsibility to provide appropriate assessment materials and translation resources.
- Can students with disabilities and an IEP receive EL support? Yes. However, it is not the role of special education to teach English as a second language. A student that qualifies for EL services may also receive special education support if the IEP Team determines that both are appropriate and necessary in order for the student to access the general education curriculum.
- Can EL staff be used to support service provision or assessment? It will be up to building principals and/or directors to determine allocation of resources and staffing. For students who qualify for special education services, the SLP can collaborate with EL staff, teachers, or interpreters in consulting regarding a student’s needs. If a student requires EL collaboration or interpreter services, the IEP Team must check the box on the special factors page indicating the language needs of a student have been considered.
(From Kent:)If a student requires EL collaboration or interpreter services, the IEP Team must check the box on the special factors, supplementary aids and assessments section of the IEP, which notes the need for supports and/or services as it relates to language needs because of limited English proficiency. If this box is checked, then the need for supplementary aids, program modifications and/or support for school personnel (such as EL collaboration and/or interpreter services, etc.) should be noted within the supplemental aids and services chart.
(Dear Colleague Letter) When conducting such evaluations, school districts must consider the English language proficiency of EL students in determining the appropriate assessments and other evaluation materials to be used. IDEA requires that the IEP team consider, among other special factors, the language needs of a child with limited English proficiency as those needs relate to the child’s IEP. To implement this requirement, it is essential that the IEP team include participants who have the requisite knowledge of the child’s language needs. See English Learners DCL.
FAQ Low Incidence Populations
- When might a student no longer require direct or consult speech-language services due to their current placement?
- When curriculum and interventions addressing language needs are embedded within their current programming, such as a student who is in a self-contained classroom, the student may not require direct or consult speech and language services due to the classroom’s curriculum (we must ensure that a student’s IEP goals align with the classroom curriculum) and their needs may be met by the student’s setting (functional language within a functional classroom).
- The ideal circumstance for discharge would be when the team—consisting of the individual with the communication disorder, the family, and the speech-language pathologist–comes to a mutual decision. The main reasons for discharge are:
- the communication disorder has been remediated or compensatory strategies have been successfully established;
- the individual or family chooses not to participate in treatment, relocates, or seeks another provider;
- treatment no longer results in measurable benefits after multiple modifications have been attempted.
- Is it appropriate to discharge a student from a speech caseload due to lack of progress?An apparent "lack of progress" is based on the assumption that the prescribed treatment goals, methods, data collection, and use are all appropriate for the individual with disabilities and their family. However, it is possible that the perceived lack of progress is actually an indication that the procedures being implemented are not well-suited to the individual with disabilities. In other words, lack of progress might indicate that the intervention is a poor fit. It is important to examine whether the intervention itself is optimal for the individual, their family, and their other caregivers and educators.
- Assuming treatment directions and methods are appropriate, it may be necessary to attempt some training and direct support for family members. The objectives of this training would likely be to make family members aware of the potential benefits of treatment participation and to clarify any confusion related to the methods used and the role of families as agents of change.
- Schepis and Reid (2003) provided a possible resource to assist with training families and other stakeholders. These authors discussed competency- and performance-based training built on adult learning principles and derived from applied research. Adopting this training approach could be an initial step in promoting the comprehensive application of communication-based treatment across settings and could lead to a dramatic change in support.
- How should we consider supporting students with speech-language needs within self-contained classrooms? If the student’s speech-language needs are being met through specialized instruction provided within the self-contained program, then speech-language services are not required. It is essential that if the student’s environment or needs change, the team must consider reestablishing direct or consult services. Supporting data must be quantified with multiple data points within the PLAAFP demonstrating that the student does not need specialized instruction provided by the SLP and that the student’s speech-language needs are being met through another service/program.
- When re-evaluating a student for ASD, who does not currently have speech and language services, but continues to meet ASD eligibility under qualitative impairments in communication, how should their communication needs be addressed in the academic setting? The student may meet the criteria for ASD and social communication needs however, their needs may continue to be met by their current placement and/or other service providers. A thorough evaluation should be conducted using both formal and informal assessment measures to assess the student’s language and social functioning to determine both the eligibility for ASD and need for services.
FAQ: Augmentative and Alternative Communication
- Is a REED required to consider AAC options for a student? A REED is not required to consider AAC options for a student unless standardized testing (e.g. Receptive/Expressive Language) is necessary in the decision-making process, then a REED should first be completed.
- When should AAC be considered for a student? AAC should be considered for any student when their speech output is not adequate to communicate everything that the student wants and needs to communicate. Additional factors to consider: the student’s frustration levels, communication partner(s) frustration levels, access to school curriculum, participation in classroom activities, ability to demonstrate knowledge to teachers, access to home and community environment, ability to interact appropriately with family and peers, and independence in developmentally-appropriate daily activities.
- When should AAC be considered as a supplemental strategy to traditional speech and language intervention? Strong consideration should be given to use of AAC to increase overall communication when a student is making slow progress in treatment, and there is a significant impact on academic and social communication due to poor speech intelligibility. Research supports that early AAC intervention can support the development of verbal expression, as well. The overarching goal is to ensure that the student has access to robust communication.
- What if the student’s SLP doesn’t feel qualified to support AAC? There are a variety of resources available to SLPs to support AAC implementation through the Wayne Assistive Technology Team (WATT) and their district Assistive Technology (AT) coach. SLP should seek additional professional development and guidance to ensure the student has access to robust communication and appropriate therapy/interventions.
- Are there AAC equipment/resources available to trial? Yes. Wayne RESA has the Wayne Assistive Technology Team (WATT) which has a lending library for our students with a moderate to severe disability. Requests can be made on their website. Alt+Shift Lending Library is available to Michigan's PK-12 public schools for short-term use of assistive technology equipment.
- If an AAC system is recommended, where should it be documented in the IEP? If the student requires any tool to communicate functionally (including light-tech communication pictures or boards), these needs should be identified in the PLAAFP, selected and included in the Supplementary Aids and Services. The AAC system can also be documented in the transition plan and/or assessments as appropriate.
- Can you write vendor or brand names of AAC systems in the IEP? AT/AAC equipment should only be described in general, non-specific terms (aka not the company’s name) when the student has access to the equipment on a permanent or semi-permanent basis (e.g. “access to a dynamic, robust vocabulary, picture-based communication support system” versus “iPad with TD Snap”). The features of the tool, that make it unique, and that are important in supporting the student should be described.
- Are measurable goal(s) and objectives needed if a student has AAC listed within the Supplementary Aids and Services? Communication goals should be developed to support the continued development of AAC skills. These goals can be discontinued when the student has demonstrated mastery in using the tool/device/strategies across all settings. See Communication Bill of Rights. The Dynamic AAC Goals Grid-2 (DAGG-2) (PDF) is a helpful tool in developing AAC focused goals.
- If the team has not started trialing AAC, but anticipate a need to explore systems and/or supports, where should this be documented in the IEP? If AAC needs are being explored altogether (e.g. it hasn’t yet been determined a need), in the anticipated needs section indicate a SETT Framework review is necessary to determine AT/AAC needs. The IEP Team must ensure that they are still collecting data on anything listed in the anticipated needs. The IEP Team should meet to design and initiate a collaborative trial plan within 30 school days. The plan should include dates for when the team will meet to review data as well as an anticipated date the trials will conclude for the purpose of making a final recommendation. Once the trial data has been reviewed and the IEP Team has made a final recommendation, the team needs to document the results of the trials and complete a summary of the recommendation. If an AT/AAC system or support is recommended, the team will need to revise the IEP to include the recommendation. Refer to FAQ 8 for how to document a recommended AAC system in the IEP.
- If the team is still trialing systems and/or supports through the SETT Framework, but need additional time to gather more data, should those systems/supports be written into the IEP?
- If it is determined that the student needs AAC but the specific system/support(s) are not yet identified and the box is checked, you can include the completion of the SETT Framework Review right within the SAS table because you’ve already determined some type of AAC is needed. You could list “SETT Framework Review is necessary to determine specific AT/AAC needs.”
- If the team knows which AAC tool will be trialed first or have an idea what solution might be a good fit for the student, it should still not be written into the IEP. There is a chance that the trial system/support won’t be the right match for the student.
- Who is responsible for providing AAC equipment? As indicated in IDEA, the student’s school system is responsible for assistive technology when it is required as a part of the student’s special education services, related services, or supplementary aids and services. This includes both the item(s) and the services required to support the item(s). The student’s family may choose to pursue private funding to obtain a personal system, with the assistance of the student’s SLP or an outside agency.
- What steps should the IEP Team take to facilitate a system going home overnight, on weekends, and breaks and into the community?
- Provide training to the parent/guardian on how to use the system and understanding the tool as a dedicated communication system
- Work with the student to become personally responsible for the system
- What is a funding report? Who can write one? The cost or partial cost of an AAC system or Speech Generating Device (SGD) may be covered by health insurance if the system is deemed a ‘medical necessity’ for the individual. The family must be an active participant in this process. Only an SLP can conduct the assessment and write the report to request an SGD.
In Wayne County, the Wayne Assistive Technology Team (WATT) provides devices for students who qualify with a moderate to severe disability while they are a student in Wayne County. If the student does not qualify for a device from WATT, the local school district is required to provide AAC as determined necessary by the IEP team.
FAQ: Speech Sound Disorders
- What do you do when a student is not making progress? It is expected various methods and strategies be employed and documented prior to service level reduction. Tracking the student’s response to the intervention provided, followed by attempts to use different approaches to intervention should be considered when making decisions to remove services. When the student has plateaued in their progress and multiple attempts have been made to redesign services, the team may discuss whether there is a lack of educational benefit. The team should make decisions about how to proceed with the input of district administrators. Refer to MSHA, 2006 SLRS-4 for more information.
- Do you consider developmental norms when treating lateralization? Lateralization of /s, z, sh, ch, j/ does not undergo spontaneous improvement with age, and therefore, should not be considered developmental. In determination of eligibility, further investigation is warranted regarding stimulability and prognosis for treatment, response to early intervening, and adverse educational effect.
- What about students with single sound errors? When single sound errors are identified, the adverse educational effect should be considered very seriously. Students who have one sound in error often experience difficulty in the classroom with social relationships, literacy skills, and vocational outcomes. In these cases, early intervention, provided either directly or indirectly with the help of parents/guardians and/or teachers, may result in improved articulation. Some districts have reported success in reducing the number of articulation referrals for students with 1-2 sound errors by providing short term intervention. It is imperative to support their educational needs by intervening when necessary, regardless of the number of speech sounds in error.
- Does dentition or tongue thrust impact speech sound production? Yes. Dentition and tongue movements should be evaluated with an oral peripheral exam, which can impact articulation and intervention. Students who have differences in dentition or tongue thrust must have a speech disorder that adversely affects school performance to be considered eligible for articulation services. See Oral Peripheral Mechanism Examination.
- When should you consider using an augmentative/alternative communication system? When a student is making slow progress in treatment, and there is a significant impact on academic and social communication due to poor speech intelligibility, strong consideration should be given to use of augmentative/alternative systems (AAC). Refer to the Augmentative and Alternative Communication accordion above.
- Do students with a history of cleft lip/palate respond to speech therapy? Approaches to treatment for articulation disorders associated with cleft palate or velopharyngeal dysfunction (VPD) will depend on whether or not speech deviations are obligatory (e.g. related to atypical anatomy and/or structural defects) or learned.
- Obligatory speech deviations that are related to true VPD or other structural deviations such as fistulas are not responsive to speech therapy and will likely require surgical intervention or other physical management.
- Learned articulation errors (e.g. compensatory errors and phoneme-specific nasal air emission) should be responsive to speech therapy.
- Do you need two standardized scores to qualify a student for an articulation impairment? You do not need to complete two standardized assessments to qualify a student SLI in the area of articulation. However, best practice is to use multiple methods and evaluation tools to support your eligibility, which may include a standardized score, observations, student/teacher/parent input, or analyzing a speech sample for intelligibility or PCC. See MARSE Guidelines, p. 35-36.
- If a student has a phonological processing disorder, would it fall under the sub area of articulation or language? Based on ASHA's updated definition of speech sound disorders as an umbrella term for errors in articulation and phonology, it is Wayne RESA’s recommendation to use the sub area of articulation for all impairments in speech sound disorders where this is the primary impairment.
FAQ: Early Intervention - Early OnⓇ - Birth to 3 years old (IDEA PART C)
- When would you consider SLI eligibility vs. ECDD eligibility for Part C MMSE (birth-3) and Part B (3-5) evaluations/ re-evaluations?ECDD may be used as a category of eligibility for MMSE services only when it is determined that the child’s primary delay cannot be attributed to another eligibility category in the MARSE. If a child meets ECDD criteria, he/she cannot meet any other criteria under any other eligibility rule. Consideration of ECDD eligibility includes:
- For an infant, toddler or preschool child, “functional performance” is an appropriate substitution for “educational performance”, which is interpreted as how the impairment adversely impacts the child’s functioning. Since infants, toddlers and preschool aged children may not be in an educational school-based setting, consideration of how the child’s ability to function as part of the child’s daily routine, including respect of the family culture, is used instead. A child’s natural environment may be his/her home, childcare setting or any other place where similar aged children without disabilities participate.
- The impact on access to and participation in functional age-appropriate activities, which cannot be differentiated among existing eligibility categories; and
- A child whose developmental delay is equal to or greater than half of the age equivalent in one or more areas of development.
- Example: If a child has a 50% speech/language delay and 50% delay in cognition, ECDD may be considered. The reason is that it’s unclear the child would qualify as a child with a Speech and Language Impairment alone; rather, the child is exhibiting deficits in cognition that constitute a more global delay.
For additional guidance for Part C (birth-3) refer to: Determination of Eligibility for Michigan Mandatory Special Education for Infants and Toddlers, Birth to age Three Early Childhood Developmental Delay Guidance (ccresa.org).
- For an infant, toddler or preschool child, “functional performance” is an appropriate substitution for “educational performance”, which is interpreted as how the impairment adversely impacts the child’s functioning. Since infants, toddlers and preschool aged children may not be in an educational school-based setting, consideration of how the child’s ability to function as part of the child’s daily routine, including respect of the family culture, is used instead. A child’s natural environment may be his/her home, childcare setting or any other place where similar aged children without disabilities participate.
- When do you consider SLI eligibility vs. ASD eligibility for Part C (birth-3) evaluations/re-evaluations?
- Example: The parent reports there are concerns on how their child interacts with siblings and others. The child care provider stated the child often plays or sits in the corner of the room by himself and is difficult to engage in activities. Evaluators observed him struggling to communicate his wants and often becoming angry. When there are global delays in communication, cognition, emotional, and social development and the child is functioning at half the chronological age, and it is not clear which area primarily affects performance, ECDD may be considered.
- The multidisciplinary evaluation team should not apply a “wait and see” approach to determine if an infant or toddler’s developmental delay or behavioral challenges meet ASD criteria. When applied, the following rationale are detrimental to the eligibility determination process:
- The family is not ready to hear the word “autism” or is uncomfortable with Autism Spectrum Disorder as the eligibility category.
- The service provider is uncomfortable telling a family that an infant or toddler meets the ASD criteria.
- The evaluation team has uncertainty assessing the impact of additional risk factors on development versus presentation of ASD characteristics.
- The evaluation team is hesitant to check the “Lifelong Disability” box on the eligibility determination form. If, after careful and comprehensive assessment, the infant or toddler fully meets the criteria for eligibility under ASD, the multidisciplinary evaluation team must provide the recommendation of ASD eligibility to the IFSP team. The practice of determining an infant or toddler meets eligibility in the categories of R 340.1710 (“Speech and language impairment” defined; determination) or R 340.1711 (“Early childhood developmental delay” defined; determination) to “wait and see” if the infant or toddler meets ASD criteria must be discontinued.
- The eligibility should best reflect the child’s primary area(s) of need/concern as it relates to functional and academic impact. Refer to: Determination of Eligibility for Michigan Mandatory Special Education for Infants and Toddlers, Birth to age Three Early Childhood Developmental Delay Guidance (ccresa.org)
- What should my frequency and duration of home visits be when creating an IFSP for a child? Early intervention teams should individually determine service frequencies, intensities, and durations based on peer-reviewed research (to the extent practicable), that are necessary to meet the unique needs of the child and the family. In determining appropriate services, the team should consider the caregiver’s learning style and need for support, social and cultural factors, and what is needed to develop a successful caregiver-professional partnership. The effects of service delivery should be monitored and services should be modified as needed to achieve outcomes.
- Who is responsible for transition planning throughout early childhood programming? If you are the child’s PSP or IEP case manager, you are responsible for facilitating communication with the child’s parent/caregiver and next transition site (e.g. LEA district rep, elementary school teacher consultant), including scheduling the meeting and organizing the necessary paperwork. Discussion about “next steps” will be directed by who is representing programming at the next level/site. The district of residence is responsible for the initial IEP.
- A child I am evaluating is 2 years, 6 months, do I complete an IFSP or an IEP? Per MARSE, early childhood special education programs/services may be provided to students with disabilities who are 2 years 6 months with an IEP. However, families must be given the option to choose an IFSP until the child turns 3. Factors to consider may include if the child is attending a community preschool, date and time of school year that the child turns 3, if the family is ready for an educational versus a family service plan, and if the child's needs are better met within a natural environment or least restrictive environment setting.
- Can a SLP provide feeding, dysphagia and/or oral motor dysfunction therapy on an IFSP/within the Early Childhood population? Yes. Refer to Special Interest Topics regarding Dysphagia in the Schools. The information included in this section is relevant and applicable to services provided within an IFSP, keeping in mind IFSP goals and services are child/family-driven with caregiver coaching for strategy implementation.
- A colleague/friend/neighbor is asking about their toddler’s speech-language development. How do they make a referral to Early On?If there are concerns about the child’s development, encourage the family to contact Early On. Referrals to Early On can be made by anyone and can be made over the phone or online. Evaluations have no cost and can be provided within the family’s home.
- Contact Early On Michigan at 1-800-Early-On or Michigan Early Childhood: Home (miearlychildhood.org) to make a referral. If they live in Wayne County, and would like to speak with the referral coordinator they can call the Wayne County referral hotline at 734-334-1393.
FAQ: Special Interest Topics
Kent ISD has compiled information relating to special interest topics in their Speech and Language Guidelines (2021) on pages 82-97. Below are Frequently Asked Questions on these special interest topic areas with Wayne RESA’s resources and guidance.
Auditory Processing Disorders
- Could a student be eligible under Section 504 with a CAPD diagnosis? Yes. A student could be found eligible as a student with a disability under Section 504 if the disability substantially limits a major life activity and requires accommodations in order to access the school environment.
Deaf and Hard of Hearing
- Who is responsible for completing a standardized language assessment? Primarily, the SLP is responsible for completing this type of assessment, due to the training and expertise in language development; however, a certified DHH teacher or DHH Teacher Consultant may also conduct expressive and receptive language assessments, due to their background in language development as well.
The results of this assessment and other formative assessment data should be reviewed by all IEP team members. The student's primary language modality should be considered. For example, if a student communicates using American Sign Language, and the SLP, the DHH Teacher, or DHH Teacher Consultant is not proficient in ASL, they must use supplemental aids (i.e. ASL Interpreter) during assessments to obtain accurate results.
- What other formative assessment data should be considered? Observational data and teacher/student/parent/guardian input is needed to support an understanding of how the individual student’s type or degree of hearing loss, use of hearing technology, community, educational, and familial factors affect the overall development of the child.
- How do we determine if DHH or SLI is the most appropriate primary eligibility? MARSE defines “deaf or hard of hearing” as any type or degree of hearing loss that interferes with development or adversely affects educational performance. “Deafness” means a hearing loss that is so severe that the student is impaired in processing linguistic information through hearing, with or without amplification. The term “hard of hearing” refers to students who have permanent or fluctuating hearing loss that is less severe than the hearing loss of students who are deaf and that generally permits the use of the auditory channel as the primary means of developing speech and language skills. Conversely, MARSE defines a speech and language impairment as a communication disorder that adversely affects educational performance, such as a language impairment, articulation impairment, fluency impairment, or voice impairment. Therefore, in determining primary eligibility, the IEP Team must collaboratively determine if the student’s impairment is a direct result of the impact of the student’s hearing loss and auditory access to spoken language or a communication disorder. Additionally, the IEP Team should collaborate on the development of the Present Levels of Academic Achievement and Functional Performance (PLAAFP) as it relates to the student’s current functional hearing levels and communication impact and identify the most appropriate supports and services within the general education curriculum for purposes of optimizing student potential.
- How does this guidance apply to students receiving DHH programming through the Wayne RESA DHH Center Program and Local Programs? This document is intended to provide guidance to SLPs supporting students who are deaf and hard of hearing in local and regional programming.
- Who should be contacted if you do not have an IEP Team member with DHH certification that is qualified to complete an evaluation? Consultation on the appropriate supports required for an evaluation can be requested from Wayne RESA’s DHH support consultant (as of August 2023 this is Celeste Johnson - johnsoc@resa.net).
- What factors should be considered when determining if a student with a hearing loss should be exited from special education services completely or qualify for a 504 plan? Before exiting, changing special education services or moving to a Section 504 Plan, the IEP team which should include a DHH staff member or Audiologist, must consider the presence of adverse impact (academic, vocational, and/or social) on the student’s ability to access and make progress in the general education curriculum. Additionally, the IEP team should consider the student’s functional communication skills in the school environment, use of their hearing equipment, performance with aided communication skills, current speech production skills and ability to both monitor and self-correct errors in their speech sound production. Possible accommodations in a 504 may include, but are not limited to: strategic seating that considers the listening environment (e.g. away from HVAC noise, open doors/windows, or other excessive talkers), copies of notes or classroom materials, access to captions for instructional videos, access to sound field system in classroom, and consideration of Remote Microphone Technology (FM system) for the student’s hearing aid. Consultation on appropriate accommodations to include for a student with a hearing loss can be requested from johnsoc@resa.net.
Dysphagia
- Dysphagia is a medical issue. Does a school SLP need to address this concern within the school setting? Dysphagia treatment falls within the scope of practice of a SLP. If a student demonstrates needs in this area and an adverse impact is determined, the SLP should be part of a school-based dysphagia team.
- What is the procedure for making a referral for a clinical swallowing study? A medical evaluation and potentially a swallow study should be the first step in developing a dysphagia treatment plan. The SLP should begin by obtaining medical history and advising the parent/guardian to bring the concerns to their physician, who can refer the student for a swallow study if deemed appropriate. It will be important to obtain a release of information, so that the SLP can communicate directly with the physician or medical SLP.
- If a school-based SLP lacks competence in the area of dysphagia evaluation/treatment, how can they ethically meet the needs of a student with dysphagia? An SLP should discuss their concerns with their special education supervisor and district SLP team. There may be another SLP within the district or ISD who can provide ongoing advice or even work directly with the student if needed.
- What is the SLP’s role in developing dietary recommendations in the school setting? Dietary recommendations regarding caloric intake and types/timing of food should be developed by a medical doctor or dietitian. The SLP may play a role in ensuring that the school carries out these recommendations and may be involved in determining food consistency, feeding positioning and provision of appropriate tools.
- What should happen if the feeding/swallowing plan is not implemented by the student’s direct care team? The feeding plan should be considered part of the student’s IEP. If deemed a necessary part of the student’s educational plan, the feeding plan should be implemented with consistency and fidelity by all school personnel.
- What is the area of eligibility in which feeding/swallowing goals would be appropriate? Many students who have dysphagia or oral motor dysfunction are already receiving school services under another eligibility area (Otherwise Health Impaired, Physical Impairment, etc). If direct speech service is deemed necessary, it can be added as a service and does not require a separate eligibility area. If no eligibility area is determined and a student continues to present with swallowing/oral motor difficulties, they may be eligible for a 504 plan.
Selective Mutism
- Do all students with SM also have a speech or language impairment? Some students with Selective Mutism have subtle speech and/or language abnormalities such as receptive and/or expressive language abnormalities and language delays. Others may have subtle learning disabilities including auditory processing disorder. In most of these cases, the students have inhibited temperaments (prone to shyness and anxiety). The added stress of the speech-language disorder, learning disability, or processing disorder may cause the student to feel that much more anxious and insecure or uncomfortable in situations where there is an expectation to speak.
- What do you do if the student does not speak during the evaluation? It is possible that a student with selective mutism may not participate in formal evaluation activities; such nonparticipation may manifest as lack of oral responses and use of nonverbal responses (e.g. pointing or gesturing.) This in itself is diagnostic information regarding the student's response to social communication. If this occurs, the SLP can use supporting information to determine the student's best communication in private settings. This may include audio or video recordings from home, which offer more information than parent/caregiver descriptions. When there is a clear discrepancy between the student's communication at home and their communication in public, this may not yield scores for traditional standardized measures of speech and language but is suggestive of the overarching problem of difficulty with social language.
- How does SM impact articulation, voice, and language? Articulation, if it is able to be assessed, is typically normal in students with selective mutism. However, the presence of an articulation disorder may compound the anxiety of interacting with others. Some students with selective mutism have reported that their voice "sounds funny". The SLP may document vocal quality at the time of the initial evaluation and then reassess during intervention. Often, the altered vocal quality lessens as anxiety decreases. Receptive language skills are typically at normal levels or above normal in students with selective mutism. Subtle deficits in expressive language may be present and are theorized to be exacerbated by lack of experience in the expressive language domain.
- How does SM impact cognitive or academic abilities? Cognitive and academic abilities are typically within normal limits in students with selective mutism; however, it can be challenging to evaluate them reliably. Difficulty responding using verbal and nonverbal responses, avoidance of interacting with unfamiliar adults, and slowness to respond can lead to lower test scores and misinterpretation of the student's ability, without consideration of anxiety as a factor in performance.
- How does SM impact social skills? Pragmatic skills typically appear impaired outside the home and other familiar environments and, at times, may appear impaired in the home as well. Research is not clear as to whether or not students with selective mutism have pragmatic language deficits beyond avoiding communicating in certain circumstances outside the home setting. Social immaturity is not uncommon because the student with selective mutism has fewer social interactions and may lack social awareness. Students with selective mutism can display decreased nonverbal and verbal indicators of social engagement, such as proxemics, facial expressions, gestures, eye contact, turn taking, participation in joint activity routines, and joint attention. Home video samples are helpful in assessing social communication and variations across settings.
Secondary Students
- At the secondary level how can communication between multiple teachers/service providers be facilitated?To assess a student’s success in the general education curriculum, it is important that a formalized communication system be recognized within the building for how information will be exchanged between general education and special education staff. This system could include the following strategies:
- A consistent, single reporting form (preferably electronic that can be simultaneously edited and reviewed by all stakeholders rather than individual reporting systems)
- Directives from building leadership that general education has responsibility to provide information as requested in a timely manner
- Regularly scheduled meetings to discuss students currently being evaluated to determine eligibility or discontinuation of special education services
- When might a student no longer require direct or consult speech-language services due to their current placement? When curriculum and interventions addressing language needs are embedded within their current programming, such as a student who is in a self-contained classroom, the student may not require direct or consult speech and language services due to the classroom’s curriculum (we must ensure that a student’s IEP goals align with the classroom curriculum) and their needs may be met by the student’s setting (functional language within a functional classroom).
- How should we consider supporting students with speech-language needs within self-contained classrooms? If the student’s speech-language needs are being met through specialized instruction provided within the self-contained program, then speech-language services are not required. However, a SLP should consider supporting identified needs through providing support to school personnel as a supplementary aids and service to coach/collaborate on ensuring fidelity of speech-language skills within the program. Additionally, it is essential that if the student’s environment or needs change, the team must consider reestablishing direct or consult services. Supporting data must be quantified with multiple data points within the PLAAFP demonstrating that the student does not need specialized instruction provided by the SLP and that the student’s speech-language needs are being met through another service/program.
- Can a SLP support concerns for speech-language skills on the transition page? A SLP should collaborate with the IEP Team to identify strengths and potential needs of the student as it relates to speech-language skills and transition planning. If these identified needs do not require speech-language related service, the IEP Team could address this as an activity within the transition page of the IEP. (e.g. a student that has pragmatic needs could consult with a SLP to support preparation for a job interview)
- When is articulation therapy appropriate at the secondary level?Articulation therapy provided at the secondary level, could be considered if any or all of the following exist:
- Adverse impact on educational performance is documented and needed for transition planning to meet graduation requirements or for post-secondary outcomes
- The student is motivated to correct error sounds
- Team recognizes and acknowledges that this requires removal from the general education curriculum and that direct instruction time will be affected